By Sara McKissick
ABSTRACT
Unfortunately, childhood maltreatment and trauma are prevalent in society. As awareness grows, so does the research on the long-term effects early exposure to traumatic events has on the developing person. Socioeconomic hardships, psychopathologies, and cognitive deficiencies correlate with early childhood adverse experiences. This review will compare normal neurological activity and development to that of children who have experienced childhood trauma. It will also further explore various factors such as the level of trauma, the onset of exposure, duration or recurrence of trauma experienced. Finally, this review will examine the effects that manifest themselves in adulthood to further understand the detrimental effects of early childhood trauma. Future research is needed to further understand developmental deficiencies and to explore outside influences on the effects seen from early trauma. There are very little extensive studies on the developmental effects because it is very hard to study children consistently, let alone find children who are undergoing adverse experiences and then observe them systematically.
KEYWORDS: adverse childhood experiences, trauma, development, stress response system, mental health
INTRODUCTION
There is a growing interest in researching the developmental and psychological consequences behind early childhood trauma. Some psychopathological symptoms in adulthood, such as depression and anxiety, have been traced back to traumatic experiences in childhood.1,10 Despite the latest research on correlation between childhood traumatic experiences and the consequences in adulthood, few studies have analyzed the biological changes that occur in the developing brain of the young child who has experienced traumatic events. For the purpose of this review, childhood trauma is defined as any exposure, either witnessing or directly involved, to death, serious injury due to violence, sexual violence, or the threat of any of those mentioned. Most research studies use ACE scores, or adverse childhood experience scores, which are retrospective questionnaires about the various trauma experienced during early childhood.
An important factor when studying the effects of trauma is the biological stress response system. Stress response systems throughout biological pathways are triggered when there is a prolonged exposure to traumatic experiences.2 Normal biological development is hindered when the body is continually exposed to stressful, traumatic situations. Usually, traumatic experiences are accompanied by such overwhelming feelings of hopelessness and terror that the children cannot cope with what they are exposed to.3 Stress is defined as some kind of threat to the body’s normal physiological state, or homeostasis.4 When trauma is experienced, either once or repeatedly, the body’s stress response system becomes activated from the exposure.2 The activation of the stress systems in the body, specifically the hypothalamic-pituitary-adrenal axis, leads to hyperactivity and hypersecretion of corticotropin-releasing hormone, CRH.5 CRH is responsible for mediating the stress response and is part of a chemical chain reaction when stress is detected.2 In normal biological development, cortisol becomes activated to bring the body back down to homeostasis once a certain level of stress occurs.2
However, in those with an early onset of traumatic experiences, constant activation or extreme activation of the stress system leads to a lowering of the threshold for a response to stress.6 A lower threshold for a biological stress response means not much is needed for the body to start producing chemicals that send the body into a fight or flight response. When children are in an environment with continuous stressors from trauma, they are unable to develop proper stress responses and respond in inadequate ways. In a study of 44 adults who experienced an early childhood trauma, anxiety ratings were much higher than the ratings of a control group. 6 These findings support that those exposed to an early childhood trauma have a much lower threshold for stress and have lower levels of cortisol secreted needed to calm the body back down. The biological changes that occur after a childhood trauma lead to a chain reaction of outcomes throughout a person’s life. Studying these stress systems has led to progress about what happens on the neurodevelopmental level when the brain endures continued exposure to traumatic conditions. This review will examine research done on the neurological development of children who have not been exposed to maltreatment and compare it to preliminary findings of biological deviations seen from adverse childhood experiences. It will then further examine the long-term effects and correlations between trauma and school performance, health problems, and lifestyle later in life.
BIOLOGICAL EFFECTS OF ADVERSE CHILDHOOD EXPERIENCES
Regarding physical brain changes, there are significant differences between brains exposed to early trauma and those that were not. Children who have experienced abuse show a much smaller cerebellum and cerebrum.2 A study of 43 maltreated children found developmental alterations to the superior temporal gyrus, or the STG.7 The right portion had developed much more than the left and there was an overall increase in the amount of gray matter that covers the surface of the brain.7 A possible reason for this elevated volume of gray matter could be adaptive development from childhood trauma. In a study of 77 healthy children ages 2-6, functional magnetic resonance imaging was used to determine levels of signal intensity, connectivity, and physical maturation of the developing brain.8 Over the course of the study, the children returned every 6 months for more scans which showed that as the children developed and grew, intensity and connectivity of signaling throughout the brain became stronger.8 The increase in these signals and their increased interconnectedness are linked to possible cognitive skills like memory, facial recognition, and certain auditory cognizance.7 Those who suffer from early traumatic experiences have interpersonal triggers, such as a specific facial expression or tone of voice.7 This shows that the development of cognitive skills becomes altered upon early exposure to stress and trauma. The increase of gray matter found in this study could be due to hypersensitivity to a conditioned stimuli from the trauma or the underdevelopment of other brain areas that were stunted as a result of experienced trauma.7 Overall, alterations to the necessary functional and structural growths in the developing brain can cause neurodevelopmental disorders.2 These alterations are brought about mainly from adverse experiences formed from various factors, all affecting the extent of the detrimental alterations, which will be explored in the following section.
FACTORS AFFECTING TRAUMA LEVEL
Duration of Trauma
The duration for which the trauma is endured plays a large role in the resulting level of trauma, neurological development, and psychological outcomes. A study involving 3,754 adolescents separated traumatic experiences based on the developmental period.9 The relationship between the developmental period in which trauma was experienced and psychopathology later seen in the adolescents was analyzed. The longer the multiple traumatic experiences occurred, the greater the risk of severity and likelihood for developing internalized and externalized symptoms of psychopathologic problems.9 The outcomes based on the timing of the onset of the traumatic experiences also varied. If the traumatic experiences continue from early childhood into adolescence, then there is a much higher risk of PTSD.9 Since the trauma was repeated over many years, it is possible that very specific triggers are developed and send victims’ bodies into hyper activation of their stress response system. If the trauma is solely from early childhood, then internal and external symptoms of pathology are experienced later in life, rather than the development of PTSD.9 The possible psychopathological outcomes become more severe as the duration of trauma lengthens. If the trauma is experienced only once, specific triggers do not have the time to develop, which is a possible explanation as to why more general internal and external symptoms are seen, such as anxiety, depression, or aggressiveness. It starts to become slightly more complicated should different types of trauma be experienced simultaneously.
Polyvictimization
While duration plays a large role, there is the also high possibility of experiencing more than one kind of trauma at the same time. Those who experience multiple traumatic experiences are sometimes referred to as polyvictims.9 A common finding among several studies was that most childhood traumas co-occur with other traumas.3,10 A study was conducted to determine the prevalence of adverse childhood experiences using ACE test scores of children in the welfare system.10 ACE test scores are adverse childhood experiences tests which ask questions about how many traumatic experiences a person has experienced. 90.4% of the children studied experienced more than one traumatic event.10 Furthermore, those in areas of larger poverty are at higher risk of having high ACE scores.1,3,10 The studies go on to show what they call a “double whammy,” or dual exposure to two different types of trauma, produces a stronger negative outcome than if the child(ren) were exposed to only one.3 Since the prevalence of polyvictimization is extremely common and the chances of it are high, children who experience any adverse experience are susceptible to developing psychopathologic complications due to an automatic increase in the risk of polyvictimization.
Severity Level of Trauma
The severity of the trauma experienced, which is very closely tied to polyvictimization and duration, has a substantial influence on the effects seen in children. The level of trauma that the child is exposed to corresponds to the internalization or externalization of symptomology in psychopathologic disorders.3 According to one study, children who experience emotional trauma, either by itself or in addition to other maltreatments, later display internalizing symptoms, like depression, anxiety, or PTSD.3 Children with more exposure to physical trauma display externalizing symptoms, which are conduct related behaviors.3 This type of symptom can be seen, for example, in school aged children through various abnormal behaviors in comparison to non-traumatized peers.
As mentioned previously, the severity level of the trauma endured seems to have overlap with the other two factors mentioned. The longer the traumatic exposure, the worse the outcome; the more multifaceted the childhood trauma is, the more severe the outcome as well. It can be presumed then, that both previous factors converge and overlap into the severity of the trauma. For instance, should a traumatic experience happen only once, then there is no chance for the child to form a habitual unhealthy response. However, should it occur intermittently throughout childhood the child has an exponentially higher risk of developing detrimental habitual responses to the trauma. Likewise, should the child experience multiple traumas, such as neglect and physical abuse, the severity of the traumatic experience rises. Trauma starts to become both mental and physical. Unfortunately, the severity of trauma can only really build; there is no way to lessen the severity of a child’s trauma. Any level of severity of trauma leads to the formation of some effect seen later in the child’s life. The effects manifest themselves early in the child’s life, continuing through adulthood and amplifying the need for therapeutic intervention.
EFFECTS SEEN LATER IN LIFE
Cognitive and School Performance Problems
One of the earliest signs of childhood adverse experiences is seen once they start going to school. Developmental deficiencies resulting from childhood trauma have been found to negatively impact school performance and cognition. In a study of 30 children between the ages of 5 and 12, there were reports of lower education levels, a higher number of subsyndromal symptoms, which are symptoms that are not severe enough to warrant a diagnosis, lower cognitive performances, and lower attention spans.11 In an additional study, those maltreated before kindergarten had lower grades, more absent days from school, higher aggression, and much higher psychological and behavioral problems in high school.12 On average, kids in school who have experienced some sort of trauma before they are of school age, perform lower and have a higher number of problems than those of the same grade level who have not experienced any childhood trauma. The traumatic experiences associated with a lower income level are separation of the parents, living with someone who has been in prison, and exposure to domestic violence.13 These cognitive, social, psychological, and behavioral problems can be traced back to the skewed neurological development resulting from early adverse experiences.
Physical and Mental Health Problems
As school performance may decrease, another long-term effect frequently observed is a general decrease in physical and mental health. Most studies use retrospective ACE test scores and current physical and mental health status of participants. From retrospective ACE scores, a direct pathway can be made from adverse childhood experiences to the mental health seen in adulthood.13 A study utilizing a survey of 29,229 adults who had an average age of 48 years, found significant ties between ACE and current health problems.14 The higher the ACE scores, or the more traumas experienced, the higher the risk for tobacco use, obesity, and binge-drinking.14 Early childhood trauma commonly results in psychopathologic disorders as well. The chance of showcasing symptoms of a mental disorder statistically increase in those who have endured childhood trauma.13 Anxiety and depression are the most observed mental issues seen in adults with childhood trauma, and it is more frequent in abused girls than in boys.12 As seen in Figure 1, those diagnosed with depression, bipolar disorder, and schizophrenia have a higher likelihood of having some sort of early childhood trauma.15,16 Most likely, childhood trauma increases susceptibility to mental disorders later in life. The stress management system was not developed properly, so there is no way for abused children’s bodies to be able to properly respond to stressful situations later experienced.
Lifestyle
Experiences in school as well as the developing mental health lead to the lifestyle of any person. Following the chain reaction set off by childhood traumatic experiences, the lifestyle of a maltreated person in childhood can be greatly affected by the long-term effects. As previously mentioned, higher ACE scores have led to worse academic success and school conduct, both of which are preludes to a disadvantage in the economic success achieved in adulthood.13 Studies have shown that those with 2 or more reported ACE’s, in comparison with those with no ACE’s, have a lower income.13 Childhood trauma and abuse is more prevalent in areas with a high poverty rate, and due to the lower education level attained, persons with traumatic childhoods have more difficulty earning a substantial living and have a lower socioeconomic status. Furthermore, ACE scores also have an association with marital status. One study concluded that those who experienced having a family member in prison or separation of their parents, have more likelihood to either not marry or divorce their partners.13 Another aspect in relation to the parents is extensive literature on the strong co-occurrence of child abuse and parental domestic violence.3 Aforementioned, ACE scores have a correlation to marital status, and it’s possible they can be related to the relationships sought out by those with previous maltreatment in their childhood. It is suspected that it becomes a vicious cycle. A child is maltreated, then grows up and may not do anything about maltreatment by their partner, has a child with him or her and unfortunately, their child starts to have similar experiences to the abused parent.
CONCLUSION
Continued research on the developmental effects of childhood trauma is imperative to further understand the malleability of the neurodevelopmental process. During early childhood, important biological maturation and growth occur. Signaling connections throughout the brain and their intensities are tied to crucial cognitive abilities such as memory, facial recognition, and auditory understanding. It is the disruption of this maturation and development that lead to evident consequences seen in adulthood of those that have experienced maltreatment in their childhood. The outcomes observed later in life are affected by polyvictimization, the severity, and duration of the trauma endured. These consequences include various psychological problems, school education level obtained, health issues, and socioeconomic hardships. The more that is researched, the more that can be learned about how to properly help those inflicted with difficulties. Future research should focus more on how outside influences can counteract the effects of adverse childhood experiences. For example, how educating teachers on trauma and triggers, having a support system in the community, and implementing treatment options at different stages in survivors’ lives would benefit trauma victims.
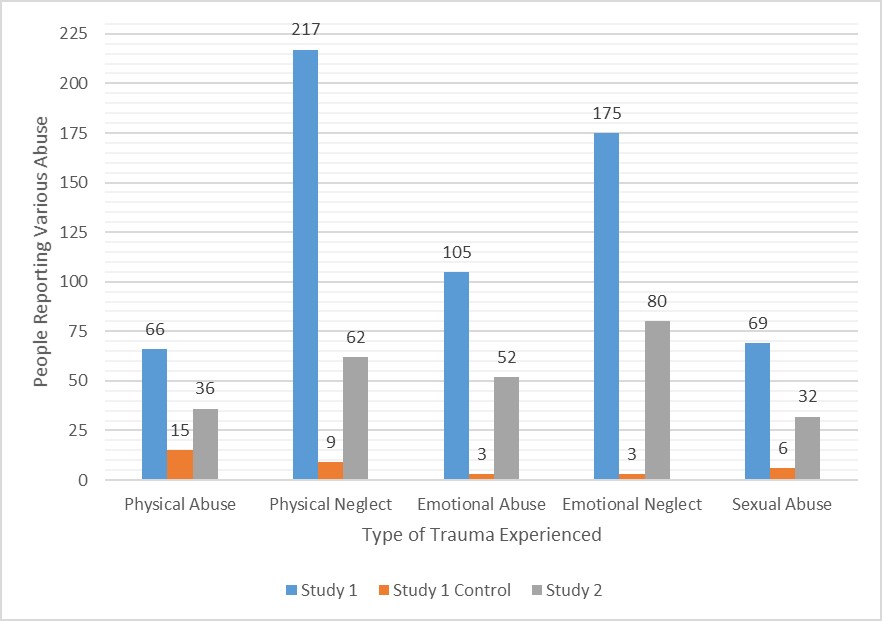
Figure 1. Prevalence of Five Different Childhood Traumas in Two Samples of Adults Diagnosed with Depression, Bipolar Disorder, and Schizophrenia. The first study, “Study 1,” had 679 individuals (N=679).15 229 of the individuals were diagnosed with depression, 102 individuals were diagnosed with bipolar disorder, and 216 individuals were diagnosed with schizophrenia.15 The second study, “Study 2,” had 129 individuals (N=129).16 60 of participants were diagnosed with depression, 17 were diagnosed with bipolar disorder, and 28 were diagnosed with schizophrenia.16
REFERENCES
- * Kaufman, J.; Plotsky, P., M.; Nemeroff, C., B.; Charney, D., S., Effects of early adverse childhood experiences on brain structure and function: clinical implications. Biological Psychiatry 2000, 48(8), 778-790.
- * De Bellis, M.; Zisk, A., The biological effects of childhood trauma. Child and Adolescent Psychiatric Clinics of North America 2014, 23(2), 185-222.
- Rosen, A.; Handley, E.; Cicchetti, D.; Rogosch, F., The impact of patterns of trauma exposure among low income children with and without histories of child maltreatment. Child Abuse & Neglect2018, 80, 301-311.
- * McEwan, B., The neurobiology of stress: from serendipity to clinical relevance. Brain Research, 2000, 886(1-2), 172-189.
- Heim, C.; Newport, D., J.; Mletzko, T.; Miller, A., H.; Nemeroff, C., B., The link between childhood trauma and depression: Insights from HPA axis studies in humans. Psychoneuroendocrinology 2008, 33(6), 693-710.
- Hengesch, X.; Elwenspoek, M., C.; Schaan, V., K.; Larra, M., F.; Finke, J.; Zhang, X.; Bachmann, P.; Turner, J., D.; Vögele, C.; Muller, C., P., Blunted endocrine response to a combined physical-cognitive stressor in adults with early life adversity. Child Abuse & Neglect 2018.
- De Bellis, M., D.; Keshavan, M., S.; Frustaci, K.; Shifflett, H.; Iyengar, S.; Beers, S., R.; Hall, J., Superior temporal gyrus volumes in maltreated children and adolescents with ptsd.Biological Psychiatry 2002, 51(7), 544-552.
- Long, X.; Benischek, A.; Dewey, D.; Lebel, C., Age-relation functional brain changes in young children. NeuroImage 2017, 155, 322-330.
- Dierkhising, C., B.; Ford, J., D.; Branson, C.; Grasso, D., J.; Lee, R., Developmental timing of polyvictimization: Continuity, change, and association with adverse outcomes in adolescence. Child Abuse & Neglect 2018.
- Kerker, B., D.; Zhang, J.; Nadeem, E.; Stein, R., E.; Hurlburt, M., S.; Heneghan, A.; Landsverk, J.; Horwitz, S., M.; Adverse Childhood Experiences and Mental Health, Chronic Medical Conditions, and Development in Young Children. Academic Pediatrics 2015, 15(5), 510-517.
- Joana Bücker, J.; Kapczinski, F.; Post, R.; Ceresér, K., M.; Szobot, C.; Yatham, L. N.; Kapczinski, N., S.; Kauer-Sant’Anna, M., Cognitive impairment in school-aged children with early trauma. Comprehensive Psychiatry 2012, 53, 758-764.
- Lansford, J., E.; Dodge, K., A.; Pettit, G., S.; Bates, J., E.; Crozier, J.; Kaplow, J., A 12-Year Prospective Study of the Long-term Effects of Early Child Physical Maltreatment on Psychological, Behavioral, and Academic Problems in Adolescence. Archives of Pediatric and Adolescent Medicine 2002, 156(8), 824-830.
- Jones, T., M.; Nurius, P.; Song, C.; Fleming, C., M., Modeling life course pathways from adverse childhood experiences to adult mental health. Child Abuse & Neglect 2018, 80, 32-40.
- Font, S., A.; Maguire-Jack, K., Pathways from childhood abuse and other adversities to adult health risks: The role of adult socioeconomic conditions. Child Abuse & Neglect 2016, 51, 390-399.
- Xiea, P.; Wu, K.; Zheng, Y.; Guo, Y.; Yang, Y.; He, J.; Ding, Y.; Peng, H., Prevalence of childhood trauma and correlations between childhood trauma, suicidal ideation, and social support in patients with depression, bipolar disorder, and schizophrenia in southern China. Journal of Affective Disorders 2018, 228, 41-48.
- Rossiter, A.; Byrnea, F.; Wota, A., P.; Nisar, Z.; Ofuafor, T.; Ivan Murray, I.; Byrne, C.; Hallahan, B., Childhood trauma levels in individuals attending adult mental health services: An evaluation of clinical records and structured measurement of childhood trauma. Child Abuse & Neglect 2015, 44, 36-45.
- *secondary research articles/ reviews
Cite this article:
McKissick, S. (2019). Effects of Childhood Trauma on Neurological Development and Mental, Physical Health in Adulthood. D.U. Quark, 3(2). Retrieved from https://dsc.duq.edu/duquark/vol3/iss2/7
Download the PDF here




Leave a comment